Sponsored Content
In a recent report, Integrated Prescription Management (“IPM”) a full-service pharmacy benefit manager, announced a highlight of its award-winning customer service, responsive analytics, and innovative cost management services on behalf of 150 county clients across Texas. From cost savings to staff time, the savings offered by IPM were evident:
- Drug cost savings ranged from 15-79%*
- Staff administration time was reduced by 25%
- Attaining lower costs for generics saved 35%
Counties working with IPM will benefit from: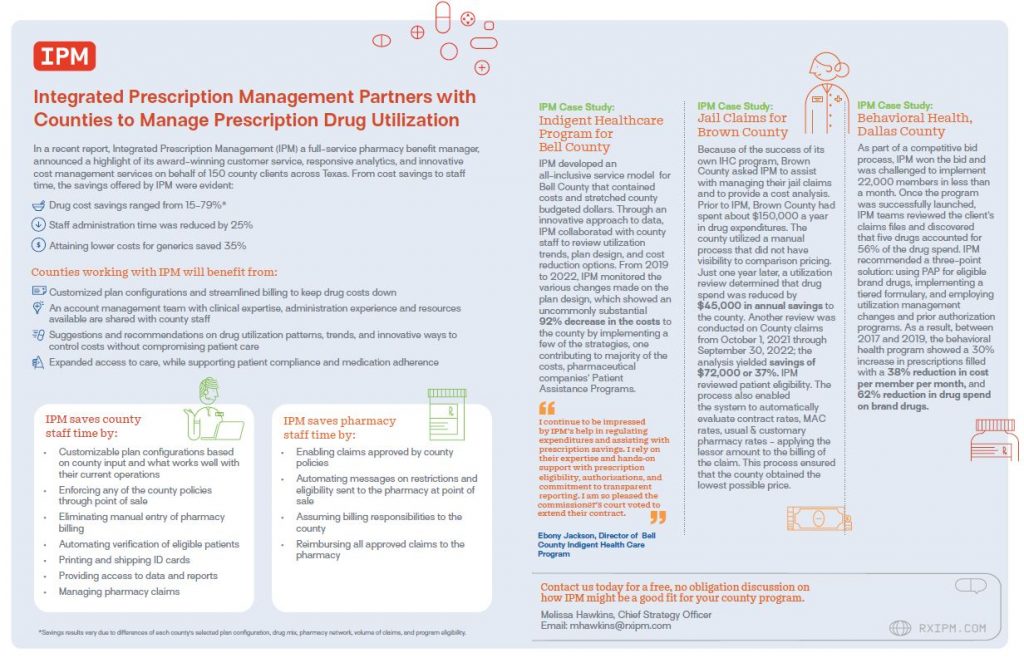
- Customized plan configurations and streamlined billing to keep drug costs down
- An account management team with clinical expertise, administration experience and resources available are shared with county staff
- Suggestions and recommendations on drug utilization patterns, trends, and innovative ways to control costs without compromising patient care
- Expanded access to care, while supporting patient compliance and medication adherence
IPM saves county staff time by:
- Customizable plan configurations based on county input and what works well with their current operations
- Enforcing any of the county policies through point of sale
- Eliminating manual entry of pharmacy billing
- Automating verification of eligible patients
- Printing and shipping ID cards
- Providing access to data and reports
- Managing pharmacy claims
IPM saves pharmacy staff time by:
- Enabling claims approved by county policies
- Automating messages on restrictions and eligibility sent to the pharmacy at point of sale
- Assuming billing responsibilities to the county
- Reimbursing all approved claims to the pharmacy
*Savings results vary due to differences of each county’s selected plan configuration, drug mix, pharmacy network, volume of claims, and program eligibility.
IPM Case Study: Indigent Healthcare Program for Bell County
IPM developed an all-inclusive service model for Bell County that contained costs and stretched county budgeted dollars. Through an innovative approach to data, IPM collaborated with county staff to review utilization trends, plan design, and cost reduction options.. From 2019 to 2022, IPM monitored the various changes made on the plan design, which showed an uncommonly substantial 92% decrease in the costs to the county by implementing a few of the strategies, one contributing to majority of the costs, pharmaceutical companies’ Patient Assistance Programs.
“I continue to be impressed by IPM’s help in regulating expenditures and assisting with prescription savings. I rely on their expertise and hands-on support with prescription eligibility, authorizations, and commitment to transparent reporting. I am so pleased the commissioner’s court voted to extend their contract.”
— Ebony Jackson, Director of Bell County Indigent Health Care Program
IPM Case Study: Jail Claims for Brown County
Because of success with its own IHC program, Brown County asked IPM to assist with managing their jail claims and to provide a cost analysis. Prior to IPM, Brown County had spent about $150,000 a year in drug expenditures. The county utilized a manual process that did not have visibility to comparison pricing. Just one year later, a utilization review determined that drug spend was reduced by $45,000 in annual savings to the county. Another review was conducted on County claims from October 1, 2021 through September 30, 2022; the analysis yielded savings of $72,000 or 37%. IPM reviewed patient eligibility. The process also enabled the system to automatically evaluate contract rates MAC rates, usual & customary pharmacy rates, – applying the lessor amount to the billing of the claim. This process ensured that the county obtained the lowest possible price.
IPM Case Study: Behavioral Health, Dallas County
As part of a competitive bid process, IPM won the bid and was challenged to implement 22,000 members in less than a month. Once program was successfully launched, IPM teams reviewed the client’s claims files, IPM discovered that five drugs accounted for 56% of the drug spend. IPM recommended a three-point solution: using PAP for eligible brand drugs, implementing a tiered formulary, and employing utilization management changes and prior authorization programs. As a result, between 2017 and 2019, the behavioral health program showed a 30% increase in prescriptions filled with a 38% reduction in cost per member per month, and 62% reduction in drug spend on brand drugs.
Contact us today for a free, no obligation discussion on how IPM might be a good fit for your county program.
Melissa Hawkins, Chief Strategy Officer
Email: mhawkins@rxipm.com






