Local Officials Seek Solutions
In a nationwide study on access to timely ambulance service, University of Southern Maine researchers determined that 4.5 million people in the United States live in an ambulance desert including 2.3 million people in rural counties.
An ambulance desert is defined as an area in which people are more than 25 minutes from an ambulance station.
According to the research report, Geographic Disparities in the Provision of Ambulance Services, 94.9 percent of Texas counties include an ambulance desert. The data, released in May 2023, listed ambulance deserts by state and county, included maps of ambulance deserts, and reported health care facility locations for every state with available data. The study also documented coverage gaps in the provision of ambulance services across geographic areas.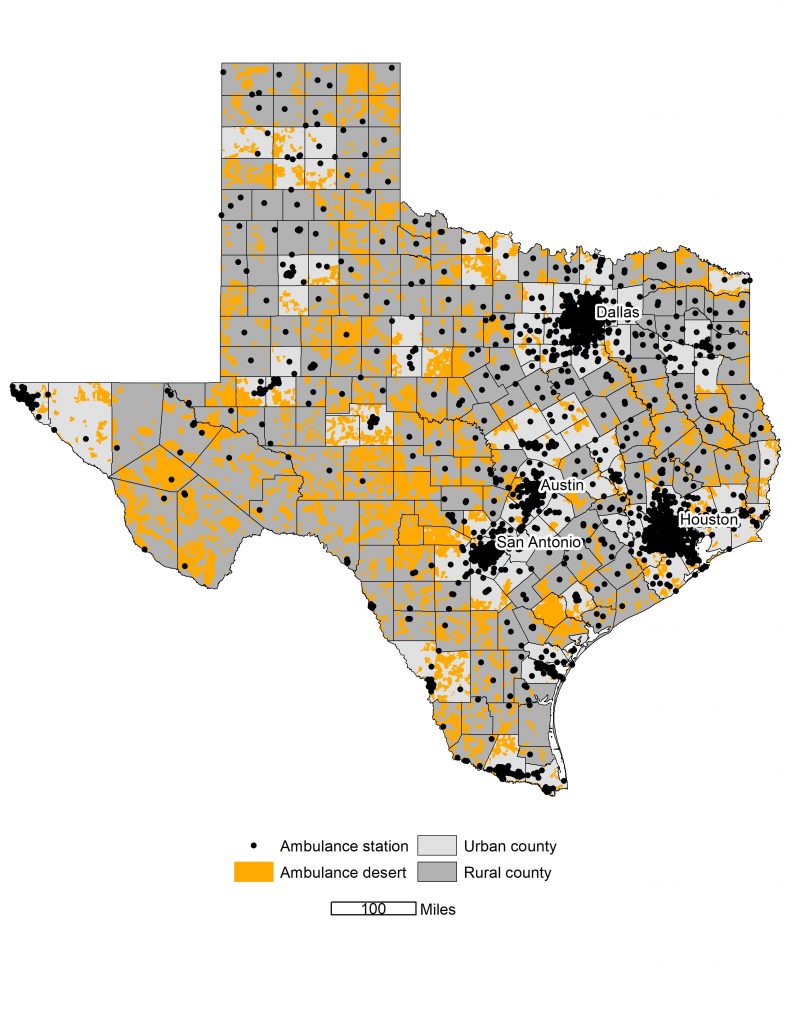
The summary of Texas rankings includes the following:
- At the top in terms of populations living in ambulance deserts.
- At the top with the highest number of rural residents living in ambulance deserts.
- At the top of states that contain several rural counties with particularly high concentrations of people living in ambulance deserts.
- In the middle of the pack when it comes to population density.
- A fairly low number of ambulance stations per thousand square miles.
- A fairly low number of ambulance stations for 100,000 people.
- The third highest number of people living in ambulance deserts.
Several factors have contributed to the challenges Texas residents face when accessing ambulance service, including hospital and clinic closures, workforce shortages, and few Medicaid increases over the last couple of decades.
According to an advocacy document produced by the Texas Emergency Medical Services Alliance, an increased transport volume stresses the system as it takes ambulances out of the community for hours due to the lengthy travel to the closest hospital, https://bit.ly/3PcpAjR. Furthermore, the increase in distances requires a higher level of training and care provided by the ambulance personnel.
Mason County Commissioner Reggie Loeffler, who spent four years operating an ambulance service, pointed out that during abnormal times such as the pandemic, staffing is even more difficult to come by as many providers serve several counties. During the pandemic, primary employers were not willing to allow their EMTs to work in other counties for fear of them contracting the virus.
When asked what could provide significant relief, Loeffler said, “Without a statewide funding source, it’s hard to imagine things getting any better for access to ambulance service.”
To overcome these challenges, counties are resorting to other forms of service including air transport. For example, in addition to ground coverage, Yoakum County offers an air transport policy to its citizens for use within the county or a contiguous county.
“For $38,000 per year, our county provides an air medical policy that covers all 8,000 residents within the county or in a contiguous county,” shared Yoakum County Commissioner Tim Addison. “Residents may also purchase an expanded statewide policy for $35.”
Lamb County Judge Mike DeLoach, who has carried a paramedic certification for almost 40 years, offered a few suggestions for a county who is looking to address the issue of accessing ambulance services.
“A lot of times people think they have to use either fully paid or fully volunteer services,” DeLoach observed, “but there are ways to blend those, as we did 30 years ago.”
Lamb County started with three full-time staffers.
“As call volume increased, we took advantage of the volunteers we had and integrated them into our system,” DeLoach explained.
Another way to approach the issue is to look at a regional system, DeLoach suggested.
“Talk to your neighbors and see what they are doing and how successful they may be,” he continued. “A combined approach could be more beneficial for all communities involved.”
All agree that there is no real silver bullet to address ambulance deserts due to various reasons including the fact that Texas is not a one-size-fits-all state.
“The State of Texas is going to have to step up,” DeLoach emphasized. “They hold me to the same standards as a paramedic in Houston. I live in a different world than the EMTs in Houston, Dallas, or Travis EMS. Those guys can attend training all day while on shift, or they have paid training. I have to pay for my own training and drive a distance to get the training.
“I am not saying we need to change the criteria,” DeLoach clarified. “However, the city of Littlefield can pay a medic $45,000 a year, but Lubbock can pay $60,000. If you are a certified EMT, you are most likely going to a community who can offer more.”
DeLoach referenced recently passed Senate Bill 22, which will provide law enforcement grants.
“If we could get an influx of money from the legislature like Senate Bill 22, that would certainly go a long way to help address the problem,” DeLoach stated.
If you have success stories in your community or are faced with trying to find a viable solution for services in your county, please email Rick Thompson at R.Thompson@Allison-Bass.com and share your story.
By Rick Thompson
CJCAT Legislative Director