County-Run Programs Provide Basic, Optional Services
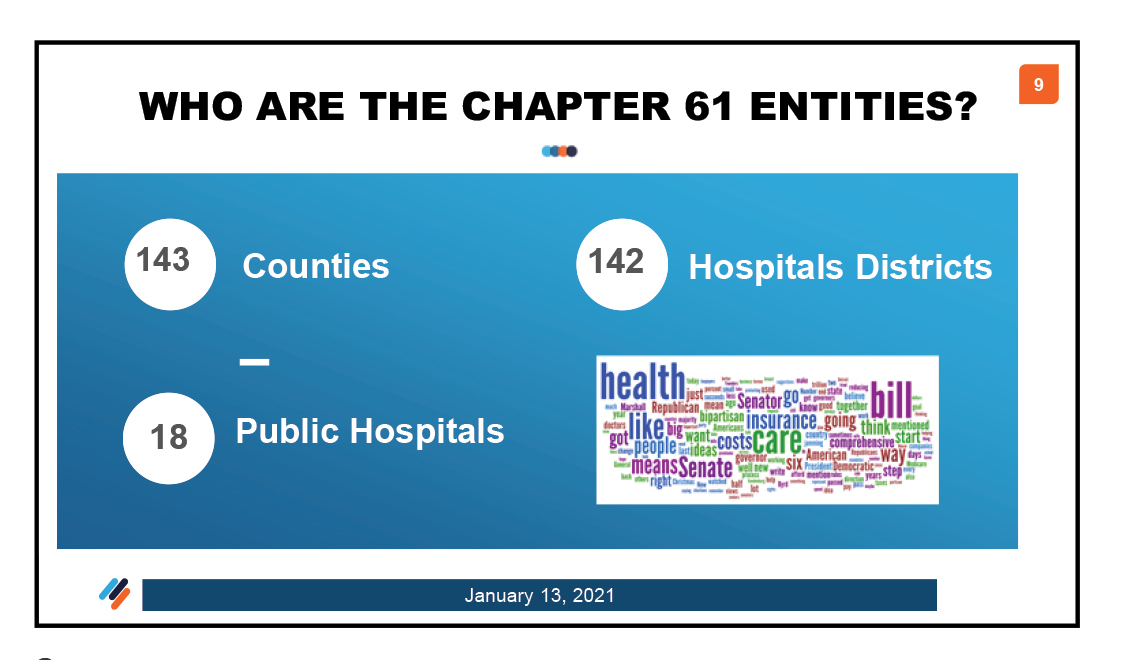
The Indigent Health Care and Treatment Act of 1985 found in Chapter 61 of the Health and Safety Code requires counties that are not completely covered by a hospital district or public hospital to provide basic health services to indigent residents through a county-run County Indigent Health Care Program (CIHCP); Texas is home to 143 county-administered CIHCPs.
On Sept. 1, 2016, the CIHCP transferred from the Department of State Health Services to Texas Health and Human Services (HHS).
Each state fiscal year, a county’s liability to provide health care services to each eligible county resident may be met in two ways or in a combination of both ways, whichever occurs first: Liability is met once a county has paid $30,000 for health care services for the eligible resident, or the county has paid for 30 days of inpatient care at a hospital or skilled nursing facility for the eligible resident, according to HHS.
Once a county spends 8 percent of its General Revenue Tax Levy (GRTL) on indigent care, the county can then request financial reimbursement through the State Assistance Fund. If the state determines the county is eligible for reimbursement, the state may reimburse the county at least 90 percent of eligible costs above the 8 percent spending level. If HHS fails to provide state funding to an eligible county, the county is not liable for payments for indigent health care services provided to its eligible residents after the county reaches the 8 percent expenditure level, confirmed HHS.
During the 86th Regular Session of the Texas Legislature, lawmakers removed former rider 120, which had been used to cap the amount of money a county could request from the State Assistance Fund, said Ty Bishop, assistant press officer with the HHS Office of Communications. Previously, an initial request could not exceed more than 10 percent of the total fund allocated for state assistance. Additional funds could be distributed as needed if no other counties required assistance. There is no longer a limit to the amount that a county may initially request, Bishop reported.
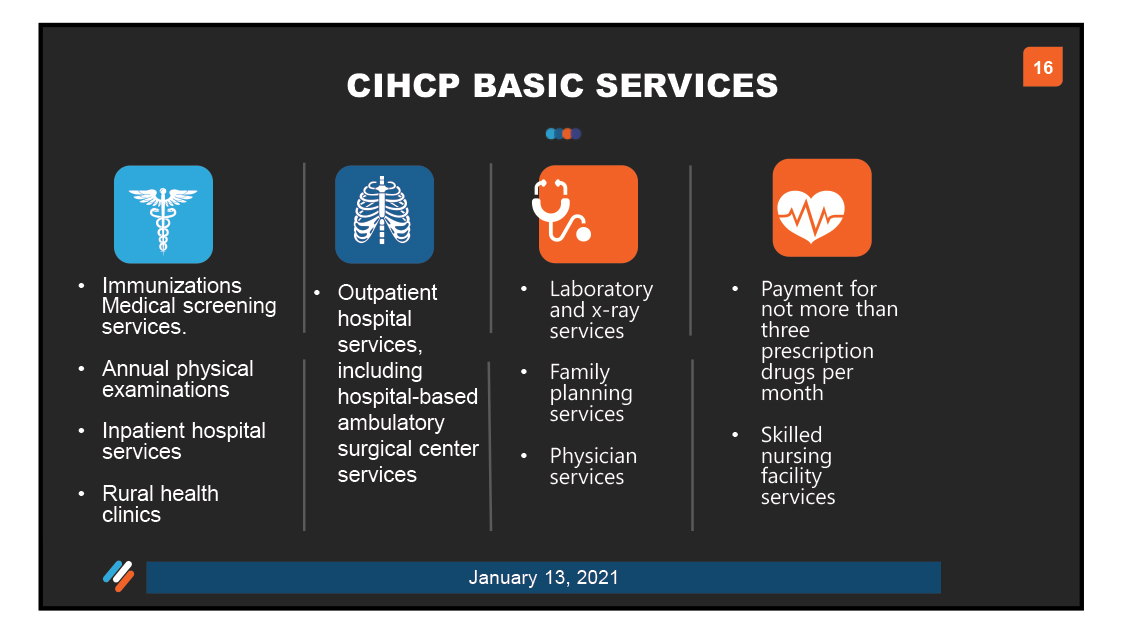
In order to qualify for state matching funds, counties are required to provide basic health care services to eligible residents and may elect to provide a number of HHS-established optional health care services. Specifically, counties must provide the following, all of which are credited to the county’s 8 percent expenditure account:
Optional health care services include the following HHS-established services:
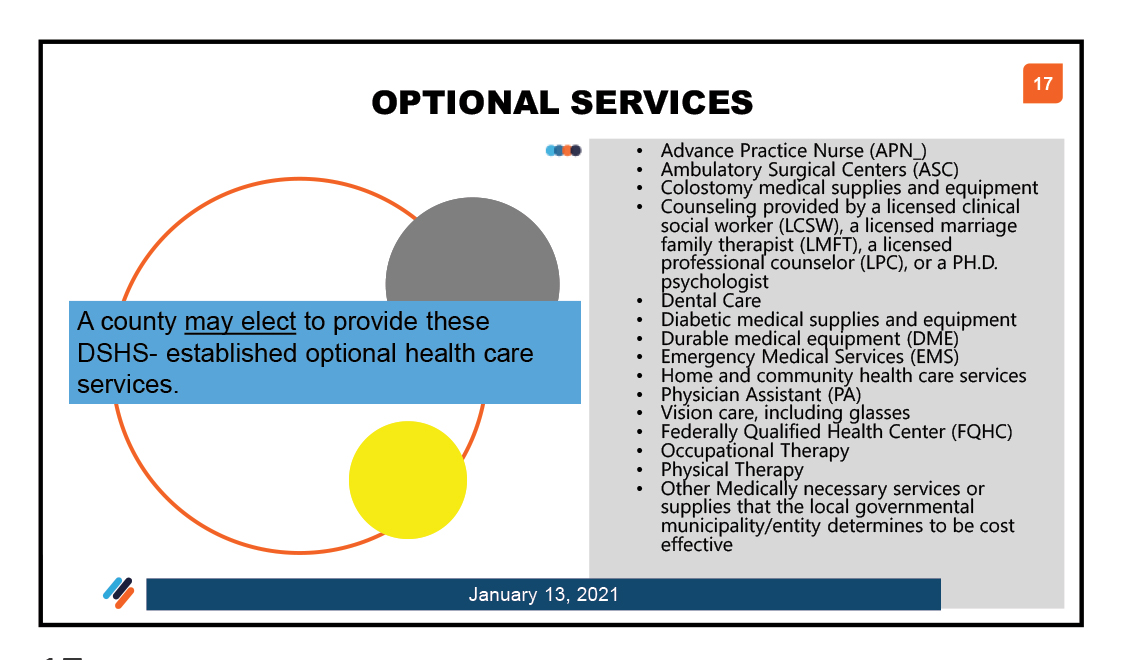
Effective March 2008, the optional health care services category was expanded to include “any other appropriate health care service that the local governmental municipality or entity deems appropriate and cost effective.” Before this addition, if a county wanted to pay for a particular service or equipment and it was not specifically in the rules, the county would not be eligible for state matching funds for that service or equipment, even if the county surpassed its 8 percent. With this change, these other expenditures can count toward the county’s 8 percent expenditure and be eligible for state matching funds.
The 83rd Texas Legislature addressed indigent health care expenditures associated with county jail inmates. House Bill 2454 amended the Health and Safety Code to authorize a county to credit an expenditure on health care services for an inmate of a county correctional facility toward the county’s 8 percent. Counties may credit expenditures for eligible residents from other counties who are inmates in their county jail. HHS developed a new, simplified application form that counties may use to determine the eligibility of inmates who are in their county jail – Form 100A.
1115 Waiver
In December 2011, Texas received approval from the Centers for Medicare and Medicaid Services for a waiver that allows the state to expand Medicaid managed care while preserving hospital funding, provides incentive payments for health care improvements, and directs more funding to hospitals that serve large numbers of uninsured patients. The Texas Health Care Transformation and Quality Improvement 1115 Demonstration Waiver, referred to as simply the 1115 Waiver, replaced the Upper Payment Limit program.
HHS has described the 1115 Waiver as an opportunity for counties to examine their current health care delivery systems and explore partnerships within their communities to help their indigent populations.
On Jan. 15, the Texas Health and Human Services Commission (HHSC) received federal approval for extending the 1115 Waiver to Sept. 30, 2030.
Counties may include 1115 Waiver intergovernmental transfer payments toward state assistance eligibility up to 4 percent of the GRTL, reported Jim Allison, general counsel of the County Judges and Commissioners Association of Texas However, there are three required findings under Section 61.036(e).
- The Commissioners Court must determine that the expenditure fulfills the county’s obligations to provide indigent health care under Chapter 61;
- The Commissioners Court must determine that the amount of care available through participation in the waiver is sufficient in type and amount to meet the requirements of Chapter 61; and
- The county must receive periodic reports from health care providers that receive supplemental or incentive payments under the 1115 Waiver that document the number and types of services provided to those eligible to receive services under Chapter 61.
For more information on the 1115 Waiver, see the related story on page 15. For more information on HHS and CIHCPs, go to https://hhs.texas.gov/services/health/county-indigent-health-care-program.